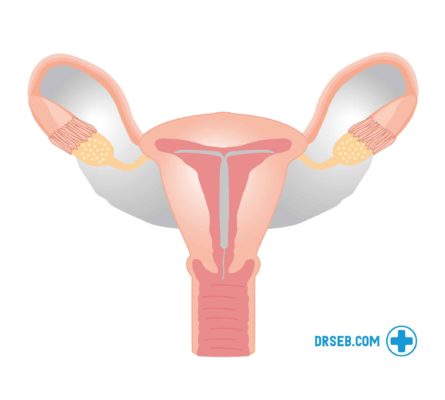
The intrauterine device (IUD) is a small copper coil that is inserted into your uterus. The device is designed to sit in the womb somewhere between 5-10 years and work through emitting copper into the womb, which changes the cervical mucus and makes it hard for the sperm to get through and for eggs to attach.
The coil is giving you a protection of 99% and is a good solution for someone who can’t or does not want to have hormonal contraceptives or don’t want to have to think about contraception for prolonged periods. It is one of the contraceptive methods that give the highest level of satisfaction for the user.1
What’s on this page?
The first forms of IUDs were created in the early 1900s, with designs that were more likely to cause infections. The method has since greatly developed, with the copper IUD that we know today first developed in the 1960s. Today, about 7% of the sexually active female population use this form of contraception.2
How does the coil work?
The coil is a T-shaped device that is made out of copper and plastic. The copper is wrapped around the plastic T, which is approximately the size of a match measuring approximately 3,6 cm long and 3,2 cm wide. When inserted, it will sit on the top part of the uterus, with the wings holding it in place.
The coil works in a few different ways to avert pregnancies:
- When inserted, the copper will act through damaging any sperm that would come into the uterus. The copper emitted is toxic to the sperm cells, which will not only inhibit their movements and make it harder to join an egg but gradually destroy them as they are passing through.
- Additionally, the coil will cause the uterus and fallopian tubes to produce a fluid that is also toxic to the sperm.
- Research suggests that it will also alter the cervical mucus, which makes it hard for an egg to attach to its wall and further develop. Though if an egg already has been attached, there is no effect on it.
The coil can be used as a form of emergency contraception within 5 days of unprotected sex. It is seen as the most efficient form of emergency contraception, although it might not be practically viable for everyone to insert a coil on short notice.
Once the device is removed, the reproductive function is reestablished as usual.
Alternative IUDs
The IUD’s also come with gold and silver coils. They are also produced in different shapes – there is one U-shaped coil and one that will form a spherical shape once inserted. These are more common abroad than in the UK.
Intrauterine devices that are emitting hormones, called Intra Uterine Systems, are also produced but they have a shorter life span and will give similar side effects to the birth control pill or transdermal patches.
How does the procedure work?
If you want to have an IUD inserted, you should book a time through a contraception clinic, GUM-clinic, your GP or clinic servicing young people. The procedure in itself normally takes about 5-10 minutes.
You will be placed in a gynaecological chair, where the practitioner might perform a preparatory examination. They will use a tool called a speculum to reach the cervix and then insert the coil. The wings of the device are flexible so that it will easily slide in.
The experience of the insertion varies greatly between individuals. Statistics show that women that have had a baby are less likely to experience pain during this procedure.3 Any pain during the procedure is caused by the device going through the cervix. Talk to your doctor about possible local anaesthetics before the procedure.
The device can be inserted during any part of the menstrual cycle and will provide contraception straight away.
After the procedure
The period after your procedure, you should stay alert and make sure that your IUD is in place and that you are not suffering from adverse effects. Some side effects are to be expected, but in rare cases, infection or rejection might occur.
The IUD has two threads attached to it, which you should be able to feel. You can check them to make sure that is it still securely in place. Do this regularly during the first month, and once in a while thereafter. If you cannot find them, the device might have moved. If this is the case, contact your GP. The same calls if the IUD would be noticeable during sex, not for you nor your partner.
About 3-6 weeks after the procedure, you will see your GP or OB-gyn again to check up on you to make sure that you are feeling alright and that the coil is in the right position.
Side effects
When the procedure is finished, it is not unusual to experience cramps that can be similar to the ones you would get during your period. Bleeding during the days following the insertion is also common. Some side effects that can come from the IUD are longer and heavier menstruation and more painful period cramps. These often disappear some months after the insertion, when the body has adjusted to the device.
Infections and other possible complications
There are a few complications that could occur after the insertion. These are:
- Pelvic infection
- Rejection
- Damage to the womb
- Ectopic pregnancy
If you have any symptoms of infection or damage (pain in your lower abdomen, a high temperature, pain when urinating and an odorous discharge) in the 20 days following your insertion you should see your GP.
Make sure that you consult your GP if you think that you might have contracted an STI, since this can cause infections and cause harm together with the coil.
Who can use this form of contraception?
Most women can use an IUD. Compared to other contraceptive methods that use hormones, this is not a risk for anyone with a high risk or embolism, has high blood pressure or smokes.
The only times when the device might not be ideal is if you would have a copper allergy or if you are pregnant already, have an STI or other infection in the womb, have had unexplained bleeding between periods or during sex, or if you have had other problems with your womb.4 Since this contraceptive method does not contain any hormones, it is alright to breastfeed whilst using the IUD.
Removing the device
Removing the device is less painful than inserting it. It is strongly recommended that you book a time with any clinic that does IUDs and book a time for the removal. Some studies claim that it might be slightly easier to take out your coil when you are on your period, but you can do it at any point of your menstrual cycle.5 The nurse or doctor will use the strings that are attached to the coil and pull it out.
Even though the process is straightforward, do not try to take it out yourself. This can result in serious damage.
If you have had sex soon before the removal of the IUD and you will have your ovulation shortly after, there is a risk of becoming pregnant since the sperm can survive in the vagina up to 5 days. Make sure to use a condom in the days before the removal, or book your time in a part of the menstrual cycle that will not put you at risk if you are not planning to become pregnant.
References: